For many individuals living with diabetes, complications such as limb amputations and organ damage are often their primary concerns. However, vision loss—another severe consequence of the disease—can come as an unexpected and devastating reality.
This was the case for Terry Quinn, a resident of West Yorkshire, who was diagnosed with diabetes as a teenager. He deliberately avoided regular medical checkups, reluctant to be labeled as diabetic, and convinced himself that the disease wouldn’t affect his daily life in any significant way.
“My biggest fear was that one day I would have to lose my leg,” he recalls. “I never thought I would lose my sight.”
It wasn’t until he began noticing a blood clot in his eye that he realized something was seriously wrong. Doctors diagnosed him with diabetic retinopathy, a condition that occurs when diabetes damages the blood vessels in the retina, leading to potential blindness. He was immediately put on laser treatment, followed by a series of injections.

Despite the medical intervention, his vision continued to deteriorate. Soon, he found himself unable to recognize his own son’s face and suffered an injury after walking into a lamppost. Eventually, he was forced to give up driving.
“I felt so helpless. I felt like I was a helpless person,” he admits.
However, a guide dog association for the blind proved to be his lifeline. They connected him with Spencer, a black Labrador, who became his guide dog and, in his words, “saved my life.” Today, Quinn dedicates his time to fundraising for guide dogs, hoping to support others facing similar struggles.
Why Early Screening for Diabetic Retinopathy is Crucial
Diabetic retinopathy is one of the leading causes of blindness worldwide, yet it is highly preventable through early screening. The UK’s National Health Service (NHS) recommends that people with diabetes undergo eye examinations every year or two, while US guidelines advise all adults with type 2 diabetes to be screened annually. However, many individuals fail to adhere to these recommendations due to cost, lack of awareness, and accessibility challenges.
“There is very clear evidence that screening can prevent vision loss,” explains Dr. Rumasa Channa, an ophthalmologist at the University of Wisconsin-Madison. However, she acknowledges that barriers such as high medical costs, logistical challenges, and communication difficulties often prevent patients from undergoing timely screening.
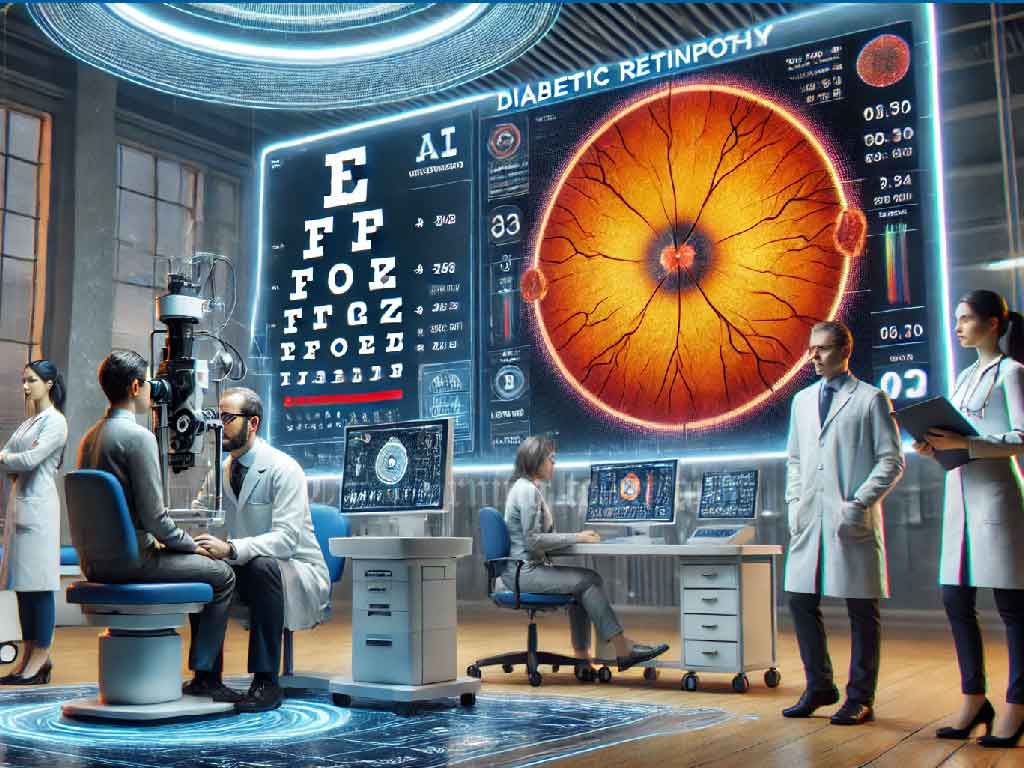
Traditional screening methods involve taking high-resolution photographs of the retina, a process known as fundus photography. Currently, these images are manually analyzed by specialists, which is both time-consuming and labor-intensive.
Dr. Channa describes the process as “a lot of repetitive work.” This inefficiency has fueled the development of artificial intelligence (AI) solutions aimed at making screening more accessible, faster, and cost-effective.
How AI is Transforming Diabetic Retinopathy Detection
AI models are proving to be a game-changer in identifying diabetic retinopathy. Since the disease follows a predictable progression, machine learning algorithms can be trained to detect it at an early stage. Some AI systems can even assess whether a patient requires a referral to an eye specialist, reducing the workload of human doctors.
One such AI-powered system has been developed by Retmarker, a health technology company in Portugal. The software scans retinal images, flags potentially problematic cases, and refers them to specialists for further evaluation.
“We usually use it as a tool to support decision-making,” explains João Diogo Ramos, the CEO of Retmarker. He believes that reluctance to embrace change is one of the key factors preventing widespread adoption of AI in medical diagnostics.
Independent studies suggest that AI-powered diagnostic tools, such as Retmarker and Eyenuk’s EyeArt, demonstrate high sensitivity and accuracy levels. Sensitivity refers to a test’s ability to correctly identify those with the disease, while specificity determines how well it distinguishes those without it.
However, high sensitivity levels can sometimes lead to false positives, causing unnecessary stress, additional medical consultations, and costly follow-up tests. Poor-quality images—resulting from dirty camera lenses, poor lighting, or operator errors—also increase the risk of misdiagnosis.
Google Health has been actively researching these challenges to refine its AI-driven diagnostic system for diabetic retinopathy. When tested in Thailand, researchers encountered significant discrepancies between real-world conditions and controlled testing environments. The primary issue was the need for high-quality images, which proved difficult to obtain in less-than-ideal settings.
Acknowledging these challenges, Google announced in October 2024 that it would license its AI model to partners in Thailand and India. The company is also collaborating with the Thai Ministry of Public Health to assess the cost-effectiveness of the technology.
The Cost Factor: Is AI Screening Affordable?
Cost remains a major consideration for AI-powered medical screening. According to Ramos, Retmarker’s service costs approximately £5 per test, although pricing varies depending on location and testing volume. The cost is significantly higher for medical facilities in the United States.
In Singapore, Dr. Daniel S. W. Ting and his team conducted a comparative study of three different diabetic retinopathy screening models. They found that traditional human-based testing was the most expensive option, while fully automated AI testing was also costly due to a high rate of false positives. The most cost-effective approach was a hybrid model, where AI performed the initial screening, and human specialists reviewed the flagged cases.
As a result, Singapore has integrated this AI-assisted model into its National Health Service Information System, set to become fully operational in 2025. However, Dr. Ting notes that Singapore’s success is partly due to its already well-established infrastructure for diabetic retinopathy screening. In other countries with weaker healthcare systems, the cost-effectiveness of AI-based screening may vary significantly.
Are AI Solutions Reaching Everyone?
Bilal Mateen, Chief AI Officer at PATH, a global health organization, highlights disparities in AI adoption. In wealthier nations such as the UK and middle-income countries like China, AI-based diabetic retinopathy screening has demonstrated strong cost-effectiveness. However, in many low-income regions, access remains limited.
“As AI advances rapidly, we need to focus more on whether its benefits are reaching everyone or are limited to a privileged few,” says Dr. Mateen. “We need more than just effectiveness data to make good decisions.”
Dr. Channa agrees, stressing that healthcare accessibility remains a pressing issue even in developed nations like the United States. She hopes AI-driven screening can help bridge the gap for underserved communities.
“We need to expand this to places where there is limited access to eye care,” she says.
However, she cautions against over-reliance on AI, emphasizing that older adults and individuals with existing vision problems should still see an ophthalmologist. While AI has shown promise in detecting diabetes-related eye diseases, it struggles with conditions such as glaucoma and myopia, which remain difficult to diagnose using current machine-learning models.
A Glimpse into the Future of AI in Eye Care
Despite its limitations, AI-driven eye screening presents an exciting opportunity to revolutionize diabetes-related healthcare. Dr. Channa envisions a future where every diabetic patient undergoes timely eye screening, reducing the risk of preventable blindness.
Meanwhile, Terry Quinn, who continues to navigate life with impaired vision, hopes that AI technology will soon become widely available. Reflecting on his own experience, he says,
“If AI had been available to detect diabetic retinopathy earlier by the time it affected me, I would have welcomed it very happily.”
The development of AI-assisted eye screening represents a major step forward in preventing blindness caused by diabetes. While challenges remain in terms of cost, accessibility, and accuracy, the potential benefits for millions of diabetic patients worldwide cannot be ignored.




